Dendritic cells (DCs) are antigen-presenting cells (also known as accessory cells) of the mammalian immune system. Their main function is to process antigen material and present it on the cell surface to the T cells of the immune system. They act as messengers between the innate and the adaptive immune systems.
Dendritic cells were first described by Paul Langerhans (hence Langerhans cells) in the late nineteenth century. The term dendritic cells was coined in 1973 by Ralph M. Steinman and Zanvil A. Cohn.[1] For discovering the central role of dendritic cells in the adaptive immune response,[2] Steinman was awarded the Albert Lasker Award for Basic Medical Research in 2007[3] and the Nobel Prize in Physiology or Medicine in 2011.[4]
The morphology of dendritic cells results in a very large surface-to-volume ratio. That is, the dendritic cell has a very large surface area compared to the overall cell volume.
The most common division of dendritic cells is "myeloid" vs. "plasmacytoid dendritic cell" (lymphoid):
1)Conventional dendritic cell (previously called Myeloid dendritic cell) (cDC or mDC)
Description: Most similar to monocytes. mDC are made up of at least two subsets:
(1) the more common mDC-1, which is a major stimulator of T cells
(2) the extremely rare mDC-2, which may have a function in fighting wound infection
Secretion: Interleukin 12 (IL-12), Interleukin 6 (IL-6), TNF, chemokines
Toll-like receptors: TLR 2, TLR 4
2) Plasmacytoid dendritic cell (pDC)
Description: Look like plasma cells, but have certain characteristics similar to myeloid dendritic cells.[5]
Secretion: Can produce high amounts of interferon-α[6] and were previously called interferon-producing cells.[7]
Toll-like receptors: TLR 7, TLR 9
The markers BDCA-2, BDCA-3, and BDCA-4 can be used to discriminate among the types.[8]
Lymphoid and myeloid DCs evolve from lymphoid and myeloid precursors, respectively, and thus are of hematopoietic origin. By contrast, follicular dendritic cells (FDC) are probably of mesenchymal rather than hematopoietic origin and do not express MHC class II, but are so named because they are located in lymphoid follicles and have long "dendritic" processes.
Life CycleIn mice, it has been estimated that dendritic cells are replenished from the blood at a rate of 4000 cells per hour, and undergo a limited number of divisions during their residence in the spleen over 10 to 14 days.[9]
The exact genesis and development of the different types and subsets of dendritic cells and their interrelationship is only marginally understood at the moment, as dendritic cells are so rare and difficult to isolate that only in recent years they have become subject of focused research. Distinct surface antigens that characterize dendritic cells have only become known from 2000 on; before that, researchers had to work with a 'cocktail' of several antigens which, used in combination, result in isolation of cells with characteristics unique to DCs
CytokinesThe dendritic cells are constantly in communication with other cells in the body. This communication can take the form of direct cell–cell contact based on the interaction of cell-surface proteins. An example of this includes the interaction of the membrane proteins of the B7 family of the dendritic cell with CD28 present on the lymphocyte. However, the cell–cell interaction can also take place at a distance via cytokines.
For example, stimulating dendritic cells in vivo with microbial extracts causes the dendritic cells to rapidly begin producing IL-12.[10] IL-12 is a signal that helps send naive CD4 T cells towards a Th1 phenotype. The ultimate consequence is priming and activation of the immune system for attack against the antigens which the dendritic cell presents on its surface. However, there are differences in the cytokines produced depending on the type of dendritic cell. The plasmacytoid DC has the ability to produce huge amounts of type-1 IFNs, which recruit more activated macrophages to allow phagocytosis.[11]
Blastic plasmacytoid dendritic cell neoplasm is a rare type of myeloid cancer in which malignant pDCs infiltrate the skin, bone marrow, central nervous system, and other tissues. Typically, the disease presents with skin lesions (e.g. nodules, tumors, papules, bruise-like patches, and/or ulcers) that most often occur on the head, face, and upper torso.[12] This presentation may be accompanied by cPC infiltrations into other tissues to result in swollen lymph nodes, enlarged liver, enlarged spleen, symptoms of central nervous system dysfunction, and similar abnormalities in breasts, eyes, kidneys, lungs, gastrointestinal tract, bone, sinuses, ears, and/or testes[21]. The disease may also present as a pDC leukemia, i.e. increased levels of malignant pDC in blood (i.e. >2% of nucleated cells) and bone marrow and evidence (i.e. cytopenias) of bone marrow failure.[13] Blastic plasmacytoid dendritic cell neoplasm has a high rate of recurrence following initial treatments with various chemotherapy regimens. In consequence, the disease has a poor overall prognosis and newer chemotherapeutic and novel non-chemotherapeutic drug regimens to improve the situation are under study.[14]
HIV, which causes AIDS, can bind to dendritic cells via various receptors expressed on the cell. The best studied example is DC-SIGN (usually on MDC subset 1, but also on other subsets under certain conditions; since not all dendritic cell subsets express DC-SIGN, its exact role in sexual HIV-1 transmission is not clear). When the dendritic cell takes up HIV and then travels to the lymph node, the virus can be transferred to helper CD4+ T-cells,[15] contributing to the developing infection. This infection of dendritic cells by HIV explains one mechanism by which the virus could persist after prolonged HAART. Many other viruses, such as the SARS virus seems to use DC-SIGN to 'hitchhike' to its target cells.[16] However, most work with virus binding to DC-SIGN expressing cells has been conducted using in vitro derived cells such as moDCs. The physiological role of DC-SIGN in vivo is more difficult to ascertain.
Dendritic cells are usually not abundant at tumor sites, but increased densities of populations of dendritic cells have been associated with better clinical outcome, suggesting that these cells can participate in controlling cancer progression.[17][18] Lung cancers have been found to include four different subsets of dendritic cells: three classical dendritic cell subsets and one plasmacytoid dendritic cell subset.[19] At least some of these dendritic cell subsets can activate CD4+ helper T cells and CD8+ cytotoxic T cells, which are immune cells that can also suppress tumor growth. In experimental models, dendritic cells have also been shown to contribute to the success of cancer immunotherapies, for example with the immune checkpoint blocker anti-PD-1.[20][21]
Altered function of dendritic cells is also known to play a major or even key role in allergy and autoimmune diseases like lupus erythematosus and inflammatory bowel diseases (Crohn's disease and ulcerative colitis).[22][23][24]
The above applies to humans. In other organisms, the function of dendritic cells can differ slightly. However, the principal function of dendritic cells as known to date is always to act as an immune sentinel. They survey the body and collect information relevant to the immune system, they are then able to instruct and direct the adaptive arms to respond to challenges.
In addition, an immediate precursor to myeloid and lymphoid dendritic cells of the spleen has been identified.[25] This precursor, termed pre-DC, lacks MHC class II surface expression, and is distinct from monocytes, which primarily give rise to DCs in non-lymphoid tissues.
Dendritic cells have also been found in turtles.[26]
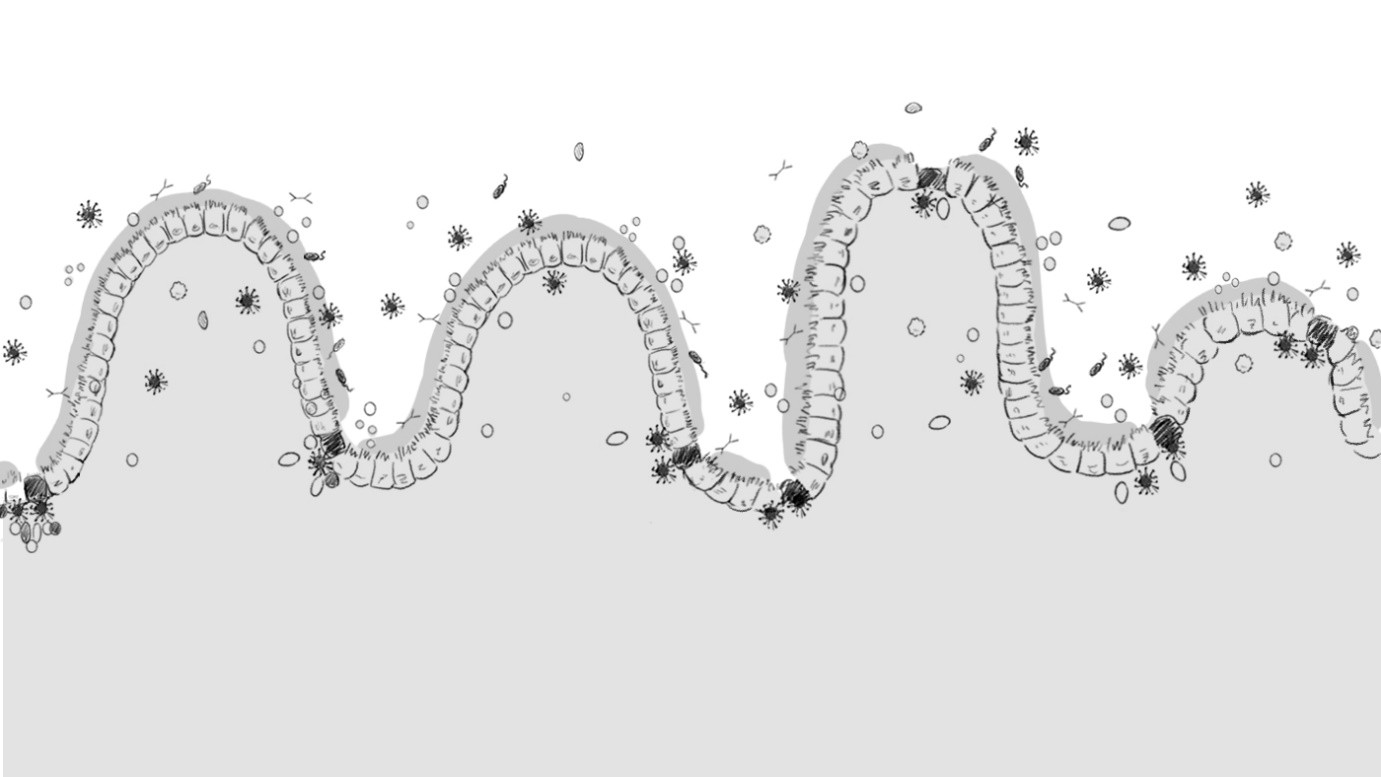
Mucosal ImmunologyMucosal immunology is the study of immune system responses that occur at mucosal membranes of the intestines, the urogenital tract and the respiratory system, i.e., surfaces that are in contact with the external environment.[27] In healthy states, the mucosal immune system provides protection against pathogens but maintains a tolerance towards non-harmful commensal microbes and benign environmental substances.[27] For example, in the oral and gut mucosa, the secretion of IgA provides an immune response to potential antigens in food without a large and unnecessary systemic immune response.[28] Since the mucosal membranes are the primary contact point between a host and its environment, a large amount of secondary lymphoid tissue is found here. The mucosa-associated lymphoid tissue, or MALT, provides the organism with an important first line of defense. Along with the spleen and lymph nodes, the tonsils and MALT are also considered to be secondary lymphoid tissue.[29] The mucosal immune system provides three main functions: serving as the body's first line defense from antigens and infection, preventing systemic immune responses to commensal bacteria and food antigens (primarily food proteins in the Gut-associated lymphoid tissue, so-called oral tolerance), and regulating appropriate immune responses to pathogens encountered on a daily basis.[30]
At birth, the neonate's mucosal immune system is relatively undeveloped, but the colonization of intestinal flora promotes its development.[31]
Because of its front-line status within the immune system, the mucosal immune system is being investigated for use in vaccines for various afflictions,[32] including AIDS[33][34][35][36] and allergies.[37]
References[1] Steinman, R. M.; Cohn, Z. A. (1973). "Identification of a Novel Cell Type in Peripheral Lymphoid Organs of Mice : I. Morphology, Quantitation, Tissue Distribution". The Journal of Experimental Medicine. 137 (5): 1142–1162. doi:10.1084/jem.137.5.1142. PMC 2139237. PMID 4573839.
[2] Banchereau J, Steinman RM (March 1998). "Dendritic cells and the control of immunity". Nature. 392 (6673): 245–52. doi:10.1038/32588. PMID 9521319.
[3] "The Lasker Foundation – 2007 Awards". Retrieved 27 November 2010.
[4] "Nobel Prize in Physiology or Medicine for 2011".
[5] McKenna K, Beignon A, Bhardwaj N (2005). "Plasmacytoid Dendritic Cells: Linking Innate and Adaptive Immunity". J. Virol. 79 (1): 17–27. doi:10.1128/JVI.79.1.17-27.2005. PMC 538703. PMID 15596797.
[6] Vanbervliet B, Bendriss-Vermare N, Massacrier C, et al. (September 2003). "The Inducible CXCR3 Ligands Control Plasmacytoid Dendritic Cell Responsiveness to the Constitutive Chemokine Stromal Cell–derived Factor 1 (SDF-1)/CXCL12". J. Exp. Med. 198 (5): 823–30. doi:10.1084/jem.20020437. PMC 2194187. PMID 12953097.
[7] Liu YJ (2005). "IPC: professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors". Annu. Rev. Immunol. 23 (1): 275–306. doi:10.1146/annurev.immunol.23.021704.115633. PMID 15771572.
[8] Dzionek A, Fuchs A, Schmidt P, Cremer S, Zysk M, Miltenyi S, Buck D, Schmitz J (2000). "BDCA-2, BDCA-3, and BDCA-4: three markers for distinct subsets of dendritic cells in human peripheral blood" (PDF). J Immunol. 165 (11): 6037–46. doi:10.4049/jimmunol.165.11.6037. PMID 11086035.
[9] Liu, Kang; Waskow, Claudia; Liu, Xiangtao; Yao, Kaihui; Hoh, Josephine; Nussenzweig, Michel (June 2007). "Origin of dendritic cells in peripheral lymphoid organs of mice". Nature Immunology. 8 (6): 578–583. doi:10.1038/ni1462. ISSN 1529-2908. PMID 17450143.
[10] Reis e Sousa C, Hieny S, Scharton-Kersten T, Jankovic D, et al. (1997). "In Vivo Microbial Stimulation Induces Rapid CD40 Ligand–independent Production of Interleukin 12 by Dendritic Cells and their Redistribution to T Cell Areas". J. Exp. Med. 186 (11): 1819–29. doi:10.1084/jem.186.11.1819. PMC 2199158. PMID 9382881.
[11] Siegal FP, Kadowaki N, Shodell M, Fitzgerald-Bocarsly PA, et al. (11 June 1999). "The nature of the principal type 1 interferon-producing cells in human blood". Science. 284 (5421): 1835–7. doi:10.1126/science.284.5421.1835. PMID 10364556.
[12] Owczarczyk-Saczonek A, Sokołowska-Wojdyło M, Olszewska B, Malek M, Znajewska-Pander A, Kowalczyk A, Biernat W, Poniatowska-Broniek G, Knopińska-Posłuszny W, Kozielec Z, Nowicki R, Placek W (April 2018). "Clinicopathologic retrospective analysis of blastic plasmacytoid dendritic cell neoplasms". Postepy Dermatologii I Alergologii. 35 (2): 128–138. doi:10.5114/ada.2017.72269. PMC 5949541. PMID 29760611.
[13] Kim MJ, Nasr A, Kabir B, de Nanassy J, Tang K, Menzies-Toman D, Johnston D, El Demellawy D (October 2017). "Pediatric Blastic Plasmacytoid Dendritic Cell Neoplasm: A Systematic Literature Review". Journal of Pediatric Hematology/Oncology. 39 (7): 528–537. doi:10.1097/MPH.0000000000000964. PMID 28906324.
[14] Wang S, Wang X, Liu M, Bai O (April 2018). "Blastic plasmacytoid dendritic cell neoplasm: update on therapy especially novel agents". Annals of Hematology. 97 (4): 563–572. doi:10.1007/s00277-018-3259-z. PMID 29455234.
[15] Cavrois M, Neidleman J, Kreisberg JF, Greene WC (2007). "In Vitro Derived Dendritic Cells trans-Infect CD4 T Cells Primarily with Surface-Bound HIV-1 Virions". PLOS Pathogens. 3 (1): e4. doi:10.1371/journal.ppat.0030004. PMC 1779297. PMID 17238285.
[16] Yang, Zhi-Yong; et al. (2004). "pH-Dependent Entry of Severe Acute Respiratory Syndrome Coronavirus Is Mediated by the Spike Glycoprotein and Enhanced by Dendritic Cell Transfer through DC-SIGN". J. Virol. 78 (11): 5642–50. doi:10.1128/JVI.78.11.5642-5650.2004. PMC 415834. PMID 15140961.
[17] Broz ML, Binnewies M, Boldajipour B, Nelson AE, Pollack JL, Erle DJ, Barczak A, Rosenblum MD, Daud A, Barber DL, Amigorena S, Van't Veer LJ, Sperling AI, Wolf DM, Krummel MF (November 2014). "Dissecting the tumor myeloid compartment reveals rare activating antigen-presenting cells critical for T cell immunity". Cancer Cell. 10 (26): 638–52. doi:10.1016/j.ccell.2014.09.007. PMC 4254577. PMID 25446897.
[18] Binnewies M, Mujal AM, Pollack JL, Combes AJ, Hardison EA, Barry KC, Tsui J, Ruhland MK, Kersten K, Abushawish MA, Spasic M, Giurintano JP, Chan V, Daud AI, Ha P, Ye CJ, Roberts EW, Krummel MF (April 2019). "Unleashing Type-2 Dendritic Cells to Drive Protective Antitumor CD4+ T Cell Immunity". Cell. 177 (3): 556–571. doi:10.1016/j.cell.2019.02.005. PMC 6954108. PMID 30955881.
[19] Zilionis R, Engblom C, Pfirschke C, Savova V, Zemmour D, Saatcioglu HD, Krishnan I, Maroni G, Meyerovitz CV, Kerwin CM, Choi S, Richards WG, De Rienzo A, Tenen DG, Bueno R, Levantini E, Pittet MJ, Klein AM (April 2019). "Single-Cell Transcriptomics of Human and Mouse Lung Cancers Reveals Conserved Myeloid Populations across Individuals and Species". Immunity. 50 (5): 1317–1334. doi:10.1016/j.immuni.2019.03.009. PMC 6620049. PMID 30979687.
[20] Moynihan KD, Opel CF, Szeto GL, Tzeng A, Zhu EF, Engreitz JM, Williams RT, Rakhra K, Zhang MH, Rothschilds AM, Kumari S, Kelly RL, Kwan BH, Abraham W, Hu K, Mehta NK, Kauke MJ, Suh H, Cochran JR, Lauffenburger DA, Wittrup KD, Irvine DJ (December 2016). "Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses". Nat Med. 22 (12): 1402–1410. doi:10.1038/nm.4200. PMC 5209798. PMID 27775706.
[21] Garris CS, Arlauckas SP, Kohler RH, Trefny MP, Garren S, Piot C, Engblom C, Pfirschke C, Siwicki M, Gungabeesoon J, Freeman GJ, Warren SE, Ong S, Browning E, Twitty CG, Pierce RH, Le MH, Algazi AP, Daud AI, Pai SI, Zippelius A, Weissleder R, Pittet MJ (December 2018). "Successful Anti-PD-1 Cancer Immunotherapy Requires T Cell-Dendritic Cell Crosstalk Involving the Cytokines IFN-γ and IL-12". Immunity. 49 (6): 1148–1161. doi:10.1016/j.immuni.2018.09.024. PMC 6301092. PMID 30552023.
[22] Baumgart DC, Metzke D, Schmitz J, Scheffold A, Sturm A, Wiedenmann B, Dignass AU (2005). "Patients with active inflammatory bowel disease lack immature peripheral blood plasmacytoid and myeloid dendritic cells". Gut. 54 (2): 228–36. doi:10.1136/gut.2004.040360. PMC 1774844. PMID 15647187.
[23] Baumgart DC, Thomas S, Przesdzing I, Metzke D, Bielecki C, Lehmann SM, Lehnardt S, Dorffel Y, Sturm A, Scheffold A, Schmitz J, Radbruch A (2009). "Exaggerated inflammatory response of primary human myeloid dendritic cells to lipopolysaccharide in patients with inflammatory bowel disease". Clin Exp Immunol. 157 (3): 423–36. doi:10.1111/j.1365-2249.2009.03981.x. PMC 2745038. PMID 19664152.
[24] Baumgart DC, Carding SR (2007). "Inflammatory bowel disease: cause and immunobiology". The Lancet. 369 (9573): 1627–40. doi:10.1016/S0140-6736(07)60750-8. PMID 17499605.
[25] Naik SH, Metcalf D, van Nieuwenhuijze A, et al. (June 2006). "Intrasplenic steady-state dendritic cell precursors that are distinct from monocytes". Nature Immunology. 7 (6): 663–71. doi:10.1038/ni1340. PMID 16680143.
[26] Pérez-Torres, A; Millán-Aldaco DA; Rondán-Zárate A (May–June 1995). "Epidermal Langerhans cells in the terrestrial turtle, Kinosternum integrum". Developmental and Comparative Immunology. 19 (3): 225–236. doi:10.1016/0145-305X(95)00006-F. PMID 8595821.
[27] "Mucosal immunology - Latest research and news | Nature". www.nature.com. Retrieved 2016-11-08.
[28] Helbert, M. (2017). Immunology for medical students (Third ed.). Philadelphia, PA: Elsevier.
[29] Helbert, M. (2017). Immunology for medical students (Third ed.). Philadelphia, PA: Elsevier, p. 84.
[30] Helbert, M. (2017). Immunology for medical students (Third ed.). Philadelphia, PA: Elsevier, p. 86.
[31] Torow, N.; Marsland, B. J.; Hornef, M. W.; Gollwitzer, E. S. (2016-09-21). "Neonatal mucosal immunology". Mucosal Immunology. 10 (1): 5–17. doi:10.1038/mi.2016.81. ISSN 1935-3456. PMID 27649929.
[32] Mucosal Immunity and Vaccines, August 2003
[33] Pavot, V; Rochereau, N; Lawrence, P; Girard, MP; Genin, C; Verrier, B; Paul, S (31 July 2014). "Recent progress in HIV vaccines inducing mucosal immune responses". AIDS. 28 (12): 1701–18. doi:10.1097/qad.0000000000000308. PMID 25009956.
[34] Bourinbaiar, Aldar S.; Metadilogkul, Orapun; Jirathitikal, Vichai (2003). "Mucosal AIDS Vaccines". Viral Immunology. 16 (4): 427–45. doi:10.1089/088282403771926274. PMID 14733732.
[35] Simerska, Pavla; Moyle, Peter M.; Olive, Colleen; Toth, Istvan (2009). "Oral Vaccine Delivery - New Strategies and Technologies". Current Drug Delivery. 6 (4): 347–58. doi:10.2174/156720109789000537. PMID 19534712.
[36] Silin, Dmytro S.; Lyubomska, Oksana V.; Jirathitikal, Vichai; Bourinbaiar, Aldar S. (2007). "Oral vaccination: where we are?". Expert Opinion on Drug Delivery. 4 (4): 323–40. doi:10.1517/17425247.4.4.323. PMID 17683247.
[37] Wild, C.; Wallner, M.; Hufnagl, K.; Fuchs, H.; Hoffmann-Sommergruber, K.; Breiteneder, H.; Scheiner, O.; Ferreira, F.; Wiedermann, U. (2007). "A recombinant allergen chimer as novel mucosal vaccine candidate for prevention of multi-sensitivities". Allergy. 62 (1): 33–41. doi:10.1111/j.1398-9995.2006.01245.x. PMID 17156339.